About Periodontal Disease
Periodontal Disease
Gum disease is one of the leading causes of tooth loss. Gum disease has two primary stages. If diagnosed and treated in the first stage, the condition can be reversed and tooth loss can usually be prevented. In order to prevent gum disease, practice good oral hygiene and visit your dentist for cleanings and check-ups twice a year.
If gum disease is detected during your visit, we will instruct you on steps regarding improved home care and recommend specialized treatment options in our office to eliminate the disease.
Gingivitis – Early Stage of Gum Disease
This stage only affects the soft tissue of the gums, and the patient may not experience any discomfort. Although the symptoms may be very mild, it is important to diagnose gum disease in this early stage before it progresses to periodontitis.
Symptoms of Gingivitis may include:
- Swollen or bleeding gums
- Bad breath or a metallic taste in the mouth
- Receding gums
- Increasing spaces between teeth
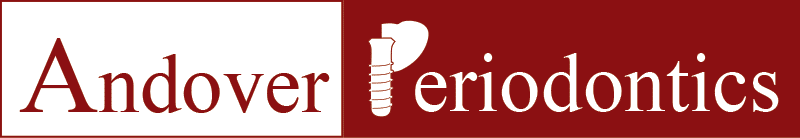
Periodontitis – Advanced Stages of Gum Disease
Periodontitis is the name for more advanced periodontal disease and if permitted to progress to this point, not only the gums are affected but the bone structures supporting the teeth will be compromised.
Without regular dental visits, symptoms may not be noticed until moderate periodontitis is present.

Healthy Gums
Firm, pink, gums attached to the teeth and supported by firm dense bone are the indicators of healthy gums and teeth that have the strong support they need.

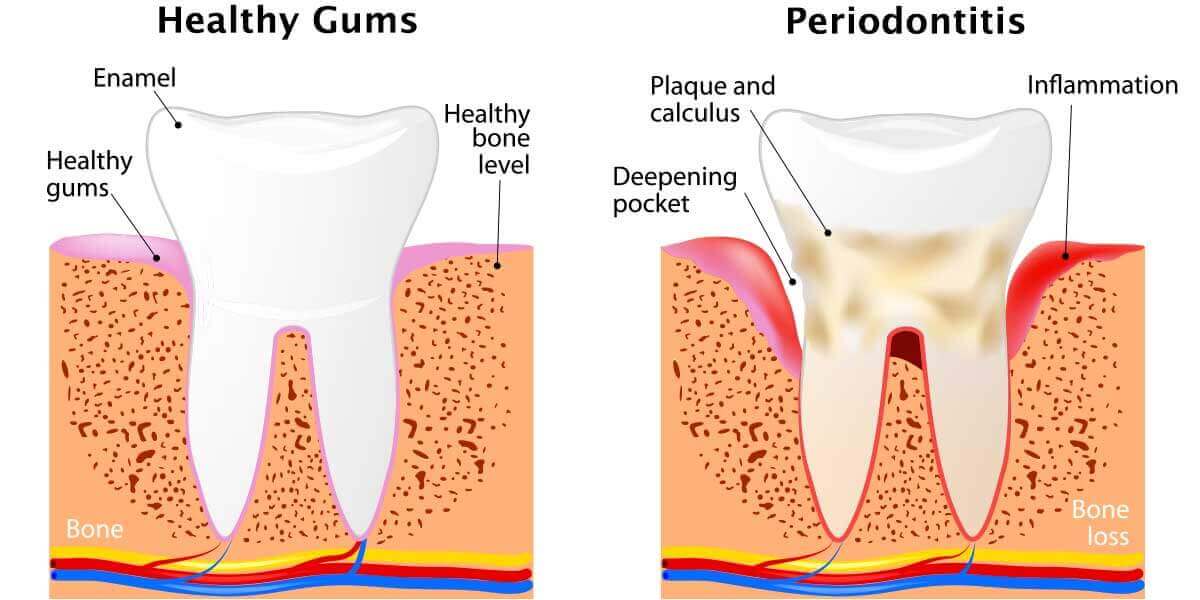
Gingivitis
A build-up of bacteria causes Gingivitis. In its early stages, inflammation around the gums is observable, with gum tissues appearing red and swollen. Gums that are easily irritated or that bleed during tooth brushing indicate the presence of Gingivitis. Removal of the plaque buildup is necessary to prevent the development of gum disease.
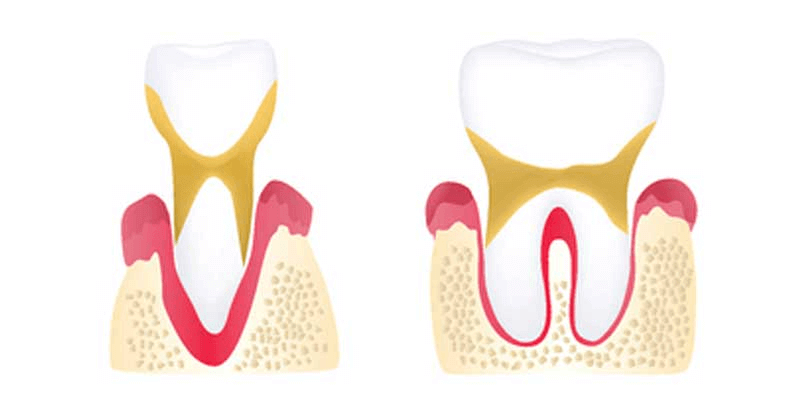
Early Periodontitis
As the gums become more inflamed, they start to pull away from the teeth, forming spaces known as periodontal “pockets.” Food, bacteria, and plaque begin to collect in the pockets, leading to infection. The surrounding bone becomes damaged both by bacterial toxins and by the immune system’s response to infection.
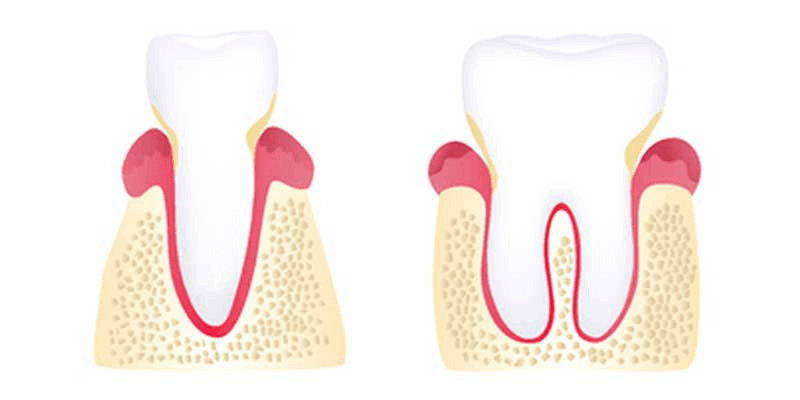
Moderate Periodontitis
The symptoms of periodontitis become more severe as inflammation spreads, and some discomfort may occur. More supporting bone is lost, teeth loosen, and the gums recede further.
Advanced Periodontitis
A major cause of tooth loss in adults, advanced periodontitis is marked by painful abscesses that are the result of the infection spreading beneath the gums.